There are two words nobody wants to hear their dentist say: root canal. In the context of your tooth’s anatomy, a root canal is simply the innermost portion of a tooth’s root, the chamber that contains the soft pulp full of nerves and blood vessels. But if your dentist is talking about a root canal, it’s probably because that pulp is damaged or infected and needs to be removed in a procedure also called a “root canal.”
You need a root canal procedure if the pulp inside a tooth has become infected or inflamed, most often as a result of an advanced cavity or other trauma. Teeth in this condition are usually experiencing persistent pain or are overly sensitive to touch, heat, or cold.
A thorough examination by a dentist will be needed to know for sure if a root canal is necessary. X-rays will probably be taken.
What are the signs that I might need a root canal?
Any dental pain is a cause for concern and should be investigated by a dentist. Dental pain can be caused by many things, tough, not just infected roots. But do you have spontaneous pain that comes on like a wave? Is the pain triggered when you change positions, such as when you bend over or lie down? Is the pain persistent? You might need a root canal.
Other warning signs include:
- Swollen, tender, or darkened gums
- Pimple-like bumps or fistula on the gums
- Lingering sensitivity to hot or cold
- A chipped or cracked tooth
- A large cavity
- An abscess
What is the purpose of a root canal?
Once the pulp of a tooth has become exposed and infected, there is no way to reverse the infection. A root canal — the removal of the pulp from the root — is the least invasive way to save the tooth and potentially give it many more years of effective use.
Is a root canal absolutely necessary?
If you want to save a tooth with an infected root, a root canal procedure is necessary. The pulp inside a tooth cannot be treated with antibiotics, and the root canal will not heal itself at this point no matter how well you start taking care of your oral hygiene.
What happens if you don’t get a root canal?
Failing to treat infected tooth pulp will allow the infection to spread from the tooth to the gum and the bone. Painful dental abscesses can form, with the associated risk of life-threatening stroke, heart attack, and sepsis.
What are the alternatives to a root canal?
Your dentist will want to be conservative in your treatment — that means saving as much of the existing structure of your mouth as possible with the minimum amount of disruptive work. In the case of infected dental pulp, a root canal procedure — likely accompanied by a crown — qualifies as the most conservative option.
The only alternative to a root canal is to extract the tooth entirely and replace it with a dental implant or bridge.
What is a root canal procedure like?
The good news is that root canals are much better than their reputation. Modern endodontic tools and techniques are designed to make root canals easy and painless. You will receive a local anesthetic to make you numb to the procedure, so you shouldn’t feel any pain. The dentist will create a small hole on the surface of your tooth and will then use small instruments to remove the infected pulp. After the pulp is removed, the dentist will disinfect the empty root canal and then fill it with rubberlike gutta-percha.
A tooth that has been through a root canal procedure is more prone to cracks and fractures, so a dental crown on the tooth will likely be recommended to strengthen it and prevent future damage.
How long will a tooth last after a root canal procedure?
Root canal procedures have a high success rate. The success of any particular root canal depends on many factors, especially the condition of the tooth at the time of treatment. A tooth with relatively minor initial damage will have a better chance of long-term survival. Some numbers:
- 98% of root canals last one year.
- 92% of root canals last five years.
- 86% of root canals last ten years or longer.
- Molar root canals performed by endodontic specialists have a 5% higher survival rate after ten years than those performed by general dentists.
What happens when a root canal fails?
Although most root canal procedures add many problem-free years of life to a tooth, there are occasional complications. Sometimes additional roots are undetected and unintentionally left behind, leading to continued pain after the procedure. Or leakage at the newly seated crown or through undetected hairline cracks in the tooth can lead to bacterial reinfection.
If discomfort persists two weeks after your procedure, make an appointment with your dentist to have it checked.
How do you avoid needing a root canal?
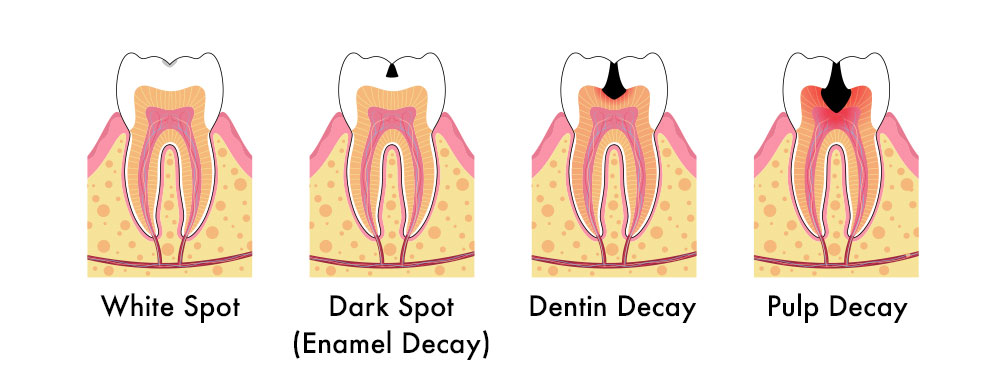
The best treatment is always prevention. Practicing good oral hygiene is the key to avoiding the need for root canal procedures. Brush your teeth at least twice a day, for two minutes each time, and floss once a day. Catch cavities early — before they work their way through the enamel and the dentin to the pulp — and keep up with visits to the dentist and dental hygienist at least twice a year. Also:
- Be careful with hard foods (hard candy, olive pits, nuts, ice, etc). See your dentist right away if you’ve cracked a tooth.
- Wear a mouth guard at night to prevent damage from grinding and clenching.
- Wear a mouth guard while playing sports.
- If you’ve got any tooth pain, see your dentist sooner rather than later. Don’t give damage a chance to progress to something worse!
REFERENCE
JOE: https://www.jendodon.com/article/S0099-2399(16)00169-2/fulltext




